The “ABCs” of Medical Technology Reimbursement in a Hospital OUTPATIENT Setting
Larry Yost | August 1, 2023 | Blog Post
In the United States, Medicare’s payment system for procedures performed in a hospital outpatient setting differs significantly from the system for inpatient payments (see my last blog post). Outpatient care includes services or procedures performed for patients whose hospital stay does not qualify to be considered an inpatient stay. In an outpatient setting hospitals bill CPT codes on a “per procedure” basis. Unlike the inpatient setting, ICD-10 codes do not directly impact payment for outpatient procedures.
While payment for patient services and procedures performed in an inpatient setting is based on single DRG payment that is determined by a combination of an admitting diagnosis (ICD-10-CM), any procedures performed (ICD-10-PCS), and the presence or absence of any qualifying complications or comorbidities, hospitals can potentially receive multiple payments for individual patients when several services and procedures are performed in an outpatient setting. The outpatient payment(s) are determined by which Ambulatory Payment Classification or APC the billed CPTs group to.
While the payment system for Ambulatory Surgery Centers (ASCs) also utilizes APCs, Medicare payment amounts are typically 40% to 50% less when performed in this setting. Procedures performed in physician office extensions or procedure centers which are not certified ASCs are reimbursed based on the Medicare Physician Fee scheduled. The idiosyncrasies of the latter will be covered in a future blog.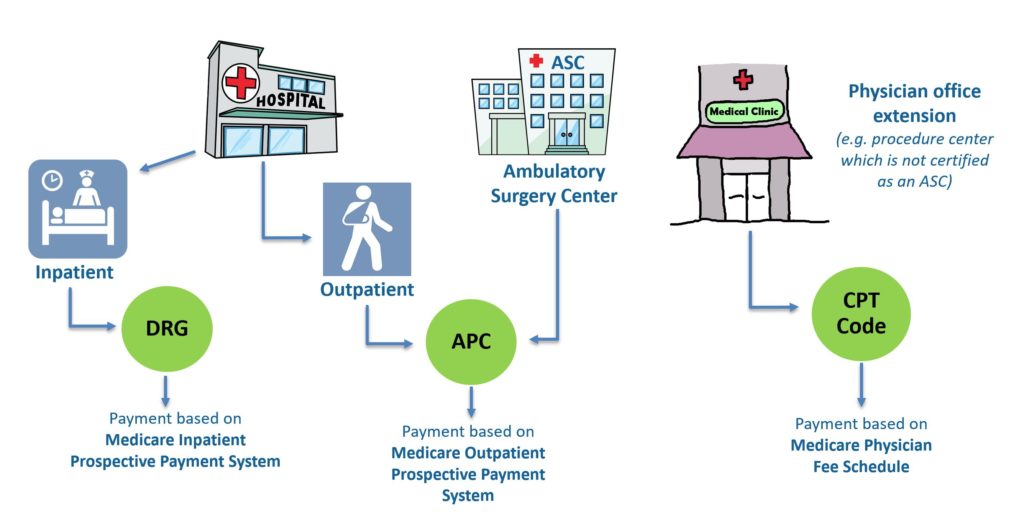 While the above provides a basic overview of Medicare reimbursement system for services and procedures performed in a hospital outpatient (and ASC) setting, there are some important caveats and nuances which should be noted.
While the above provides a basic overview of Medicare reimbursement system for services and procedures performed in a hospital outpatient (and ASC) setting, there are some important caveats and nuances which should be noted.
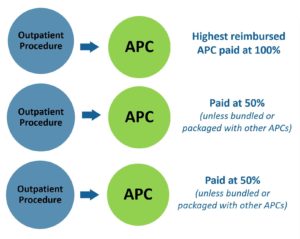 If multiple procedures and services are performed during the same hospital outpatient admission, the highest reimbursement procedure is paid at 100% of the Medicare payment rate and the remainder are paid at 50% of the Medicare payment rate. This is known as the “multiple procedure reduction” rule.
If multiple procedures and services are performed during the same hospital outpatient admission, the highest reimbursement procedure is paid at 100% of the Medicare payment rate and the remainder are paid at 50% of the Medicare payment rate. This is known as the “multiple procedure reduction” rule.
- Beginning on January 1, 2015, Medicare began using comprehensive APCs (C-APCs) which bundle certain procedures with all related ancillary services which are commonly provided/performed in conjunction with a primary procedure (e.g. imagining services, gaining vascular acces). If a CPT code maps to a C-APC, there is only a single payment for the procedure and the associated ancillary services.
- While CPT codes describe services and procedures and NOT medical devices, Medicare has created the Transitional Pass-Through Payment program for hospital outpatient procedures which provides the opportunity for new technologies to be reimbursed if they represent a truly new category of devices (see current list of categories) and they meet specific criteria required to obtain a pass through code (link to criteria). It is important to note that pass through status is only good for approximately 2 years after which Medicare will determine if it will be incorporated into an existing APC (or C-APC) with a change in the payment rate for the APC or if it will be assigned to a New Technology APC.
Having insight on the potential impact the setting in which a new medical technology will be utilized in is important to having an understanding of how the technology impact a hospital or provider economics. Since there are differing coding, billing and payment systems and scenarios which are dependent on whether the technology is utilized in either an inpatient, outpatient, ASC, or physician office setting, identifying the most likely setting(s) where the technology will be used (or when reimbursement in one of these settings will not be conducive to adoption of the use of the technology) can influence your overall targeting and market segmentation strategy. This is especially the case during the early commercialization period when you may be still in the process of implementing your reimbursement strategy.
